When we talk about eating disorders, it’s more than likely that you’re talking about anorexia nervosa, bulimia nervosa, or binge-eating disorder.
These are the three main eating disorders (EDs) that get most media, public health, and clinical attention.
However, there is a group of people who show signs and symptoms of these EDs but don’t quite meet the specific diagnostic criteria for the “main” EDs.
We refer to this group as the Other Specified Feeding or Eating Disorders (OSFEDs).
Table of Contents
What are the OSFEDs?
Put bluntly, OSFEDs represent “the rest” – those who do not meet the specific criteria for the three main EDs but show clinically significant signs and symptoms of EDs.
Of course, OSFEDs are just as important and serious as all the other EDs, and they deserve just as much research, clinical and public health attention.
What about EDNOS?
OSFED was previously called Eating Disorder Not Otherwise Specified (EDNOS) in the prior DSM, and EDNOS actually captured people with binge-eating disorder among a range of other atypical presentations.
Now, the publication of latest DSM-5 ncludes binge-eating disorder as a separate diagnostic category, and has renamed EDNOS to OSFED. The result of this change meant that far fewer individuals now have an OSFED diagnosis (compared to the number of people with an EDNOS diagnosis).
What do OSFEDs look like?
There are many different “types” of OSFEDs. They don’t represent one ED, but rather a bunch of different EDs that resemble the three main EDs.
- Atypical Anorexia Nervosa: All criteria are met, except, despite significant weight loss, the individual’s weight is within or above the normal range.
- Binge Eating Disorder (of low frequency and/or limited duration): All of the criteria for BED are met, except at a lower frequency and/or for less than three months.
- Bulimia Nervosa (of low frequency and/or limited duration): All of the criteria for bulimia nervosa are met, except that the binge eating and inappropriate compensatory behavior occurs at a lower frequency and/or for less than three months.
- Purging Disorder: Recurrent purging behavior to influence weight or shape in the absence of binge eating.
- Night Eating Syndrome: Recurrent episodes of night eating. Eating after awakening from sleep, or by excessive food consumption after the evening meal. The behavior is not better explained by environmental influences or social norms. The behavior causes significant distress/impairment.
Symptoms and Consequences of OSFED
Although there are specific examples of OSFED, many people who present with OSFED display a range of different physical, behavioural, and emotional signs and consequences.
Physical
- Regular body weight fluctuations
- Stomach cramps, other non-specific gastrointestinal complaints (constipation, acid reflux, etc.)
- Menstrual irregularities
- Impaired concentration
- Anemia
- Slowed heart rate
- Dizziness
- Difficulties in initiating and maintaining sleep
- Cuts and calluses across the top of finger joints (a result of inducing vomiting)
- Dental problems, such as enamel erosion, cavities, and tooth sensitivity
- Dry skin
- Swelling around area of salivary glands
- Fine hair on body
- Cavities, or discoloration of teeth from vomiting
- Muscle weakness
- Poor wound healing
- Impaired immune functioning
Behavioural/Emotional
- Excessive focus on weight loss, dieting, and controlling food intake
- Preoccupied with weight, food, calories, fat grams, and dieting
- Refuses to eat certain foods types or food groups
- Makes frequent remarks about feeling “fat” or overweight
- Refusal to acknowledge hunger
- Binge eating and/or purging or compensatory behavior
- Appears uncomfortable eating around others
- Develops unusual food rituals
- Skips meals or fasts for long periods of time
- Disappears after eating, often to the bathroom
- Fear of eating in public or with others
- Steals or hoards food in strange places
- Hides body with baggy clothes
- Maintains excessive, rigid exercise regimen
- Withdraws from usual friends and activities
- Looks bloated from fluid retention
- Shows extreme concern with body weight and shape
- Frequent checking in the mirror for perceived flaws in appearance
- Regularly eats in secret due to shame/embarrassment
- Extreme mood swings
Key Statistics on OSFEDs
A recent large-scale epidemiological study estimated the point-prevalence of a range of different OSFEDs 1Mitchison, D., Mond, J., Bussey, K., Griffiths, S., Trompeter, N., Lonergan, A., . . . Hay, P. (2019). DSM-5 full syndrome, other specified, and unspecified eating disorders in Australian adolescents: prevalence and clinical significance. Psychological Medicine, 1-10.
Here are some of the important statistics from this study.
- 2.9% of the population met criteria for atypical anorexia nervosa
- 2.1% of the population met criteria for bulimia nervosa of low frequency
- 0.3% of the population met criteria for binge-eating disorder of low frequency
- 3.2% of the population met criteria for purging disorder
- 4.1% of the population met criteria for night eating syndrome
- 11.2% of the population met criteria for any OSFED
- Women outnumber men twofold in the prevalence of OSFED.
- The prevalence of OSFEDs doubled the prevalence of a threshold ED
Treatment for OSFED
Since there are many different types of OSFEDs, the correct treatment approach will vary depending on the presentation of the individual.
For example, OSFEDs that are characterised by binge eating and purging behaviours require a more cognitive-behavioural approach, while OSFEDs that resemble anorexia nervosa may benefit from the Maudsley-based approach (MANTRA)
Let’s dive into these two treatment approaches for OSFEDs.
Cognitive-Behavioural Therapy
CBT is a widely used therapeutic approach that aims to normalize eating behavior and modify dysfunctional attitudes held towards weight and shape 2Fairburn, C. G., Cooper, Z., & Shafran, R. (2003). Cognitive behaviour therapy for eating disorders: A “transdiagnostic” theory and treatment. Behavior Research and Therapy, 41, 509-528.
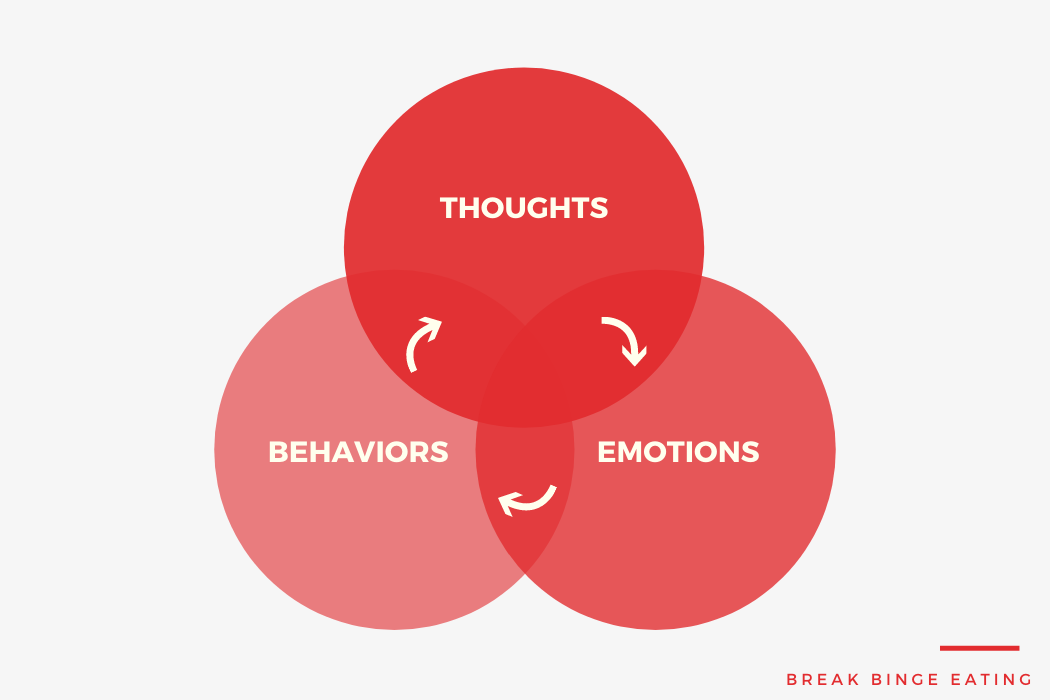
CBT is primarily concerned with the factors that maintain binge eating and purging behaviours, including extreme dieting and concerns with body weight and shape.
CBT tackles OSFED through a range of different treatment strategies, including:
- Real-time monitoring of eating patterns
- Regular, structured eating regimes
- Exposure-based exercises to feared foods
- Problem solving
- Mindfulness meditation
- Cognitive restructuring of faulty thoughts related to shape, weight, and eating
CBT has been used to effectively treat many different OSFEDs, including bulimia nervosa and binge-eating disorder of low frequency, purging disorder, and night eating syndrome.
In fact, research suggests that as many as 50% of people with OSFEDs completely recovery, with many more showing improvements in core symptoms 3Fairburn, C. G., Bailey-Straebler, S., Basden, S., Doll, H. A., Jones, R., Murphy, R., . . . Cooper, Z. (2015). A transdiagnostic comparison of enhanced cognitive behaviour therapy (CBT-E) and interpersonal psychotherapy in the treatment of eating disorders. Behaviour Research and Therapy, 70, 64-71.
MANTRA
MANTRA is another evidence-based treatment approach used primarily for younger people with OSFEDs that resemble anorexia nervosa.
MANTRA is a formulation-based treatment that is accompanied by a client workbook.
It is designed to be individually tailored to the clients presenting symptoms, personality traits, and neuropsychological profile.
MANTRA primarily focuses on targeting 4 core maintaining factors of anorexia nervosa:
- A clients thinking style
- A clients emotional/relational style
- A loved ones’ responses to the person with anorexia nervosa
- Core beliefs about the utility of anorexia nervosa in the person’s life.
Recent research shows that MATRA can be highly effective for presentations that resemble anorexia nervosa. In particular, research has shown that up to 50% of people no longer exhibit pathological thoughts, feelings, and attitudes towards food, eating, and body image 4Byrne, S., Wade, T., Hay, P., Touyz, S., Fairburn, C. G., Treasure, J., . . . Crosby, R. D. (2017). A randomised controlled trial of three psychological treatments for anorexia nervosa. Psychological Medicine, 1-11.
A Final Word
Hopefully it’s become pretty clear to you that OSFEDs are just as important as the main EDs we typically hear about.
To reinforce this statement, previous research shows that people with OSFED are just as impaired physically, emotionally, and psychologically to people with anorexia nervosa, bulimia nervosa, or binge-eating disorder 5Fairweather‐Schmidt, A. K., & Wade, T. D. (2014). DSM‐5 eating disorders and other specified eating and feeding disorders: Is there a meaningful differentiation?. International Journal of Eating Disorders, 47(5), 524-533.
We need to start talking about OSFED more often, and ensure that these individuals are not neglected in public health efforts to address EDs.
They are far from atypical!
References

Leave a Reply