Dialectical behaviour therapy (DBT) is becoming more and more popular for treating a range of mental health problems.
Originally, DBT was developed as an outpatient treatment for women with borderline personality disorder (BPD), who frequently struggle with emotion dysregulation and recurrent suicidal ideation and behaviour 1Dimeff, L., & Linehan, M. M. (2001). Dialectical behavior therapy in a nutshell. The California Psychologist, 34(3), 10-13.
Now it has been adapted for use for a range of different mental health problems, including mood disorders, substance use disorders, and eating disorders.
What actually is Dialectical Behavior Therapy (DBT)?
Dialectical behaviour therapy (DBT) is a comprehensive skills-based therapy that primarily aims to teach people a broader range of healthy coping strategies 2Lynch, T. R., Trost, W. T., Salsman, N., & Linehan, M. M. (2007). Dialectical behavior therapy for borderline personality disorder. Annu. Rev. Clin. Psychol., 3, 181-205.
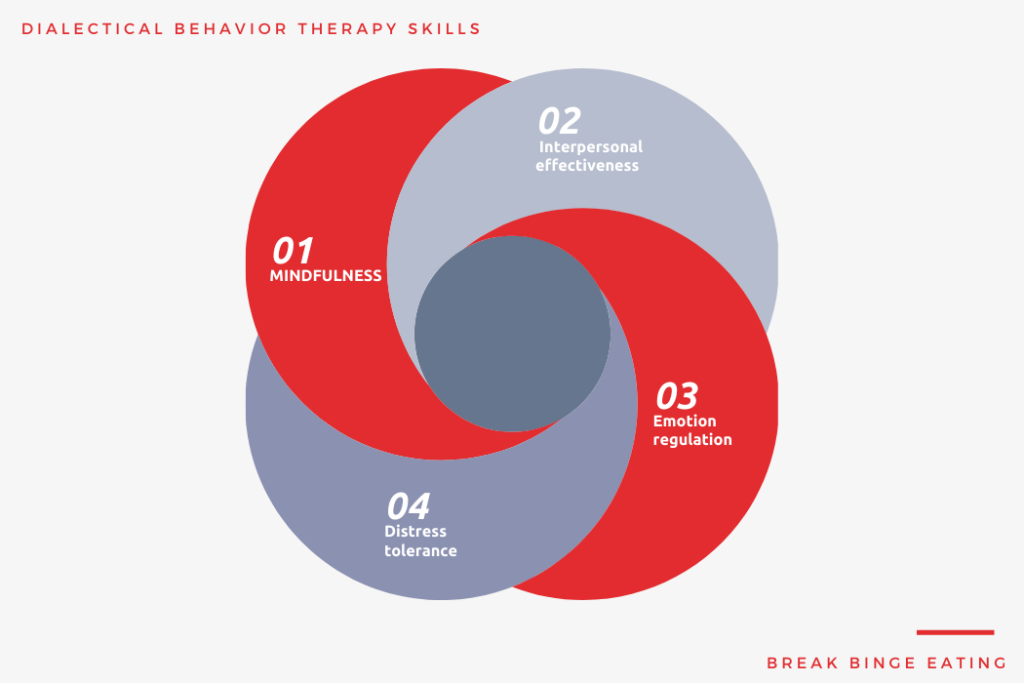
In doing so, it focuses on four major therapy skills:
- Mindfulness
- Interpersonal effectiveness
- Emotion regulation
- Distress tolerance
By focusing on these, It is considered part of the family of cognitive-behavioural therapies.
But, the format of DBT is quite different to traditional CBT. In particular, the format of DBT incorporates all of the following:
- Weekly, individual psychotherapy sessions
- Weekly group skills sessions
- 24-hour telephone consultation
- Therapist consultation team
It wasn’t soon after DBT was proven to be effective for BPD that a DBT therapy was adapted for eating disorders.
Why Adapt DBT for Eating Disorders?
DBT is based on a model that assumes that mental health problems are largely caused by an inability to handle our emotions properly 3Lynch, T. R., Chapman, A. L., Rosenthal, M. Z., Kuo, J. R., & Linehan, M. M. (2006). Mechanisms of change in dialectical behavior therapy: Theoretical and empirical observations. Journal of clinical psychology, 62(4), 459-480.
Eating disorders, and in particular binge eating and purging behaviours, fit this model nicely.
We know that various eating disorder behaviours, like binge eating and purging, are often caused by negative mood states, including sadness, loneliness, frustration, and anger.
This is because these emotions aren’t pleasant to experience, so people do the best they can to try to avoid or escape them.
Binge eating and purging behaviours offer this escape.
So, DBT tries to teach people to implement better coping strategies.
It’s important to point out that DBT isn’t used for anorexia nervosa – only bulimia nervosa and binge eating disorder.
How DBT for Eating Disorders Differs from DBT for Borderline Personality Disorder (BPD)?
The DBT treatment used for eating disorders is a little bit different to the DBT program used for borderline personality disorder.
Let’s take a look at how adapted DBT for eating disorders is different from DBT for BPD.
DBT for eating disorders combines two modalities into one modality, either a 2-hour group treatment for binge-eating disorder or a 60-minute individual session for bulimia nervosa.
DBT for eating disorders is much briefer. As opposed to the usual year-long treatment for BPD, DBT for eating disorders lasts 20 sessions.
DBT for eating disorders focuses on three rather than the four major therapy skills, including mindfulness, emotion regulation, and distress tolerance. Interpersonal effectiveness is not addressed.
DBT for eating disorders uses many different techniques to DBT for BPD, including the concept of dialectical abstinence, mindful eating, urge surfing, and alternate rebellion.
DBT Treatment: Structure, Components, and Techniques
The format of each session if the 20 DBT sessions is divided evenly.
The first half of each session is devoted to homework review and includes discussion of client diary cards and chain analyses. Clients are required to discuss how they implemented the new skills in their daily life, or any barriers they encountered that prevented them from implementing these skills.
The second half of each session is devoted toward teaching new content and practice of new skills, also known as skill acquisition.
Let’s turn our attention to some of the specific treatment techniques used in DBT.
Diary Cards
Diary cards serve the function of self-monitoring. They enable the person to closely monitor their thoughts, feelings, and behaviours associated with food and eating.
The idea is that the more a person can learn about their eating experiences, the better they’ll be able to tackle their eating disorder behaviors.
In a typical diary card, clients are expected to record the following throughout a given day:
- Ratings of the urge to binge
- Number of binge episodes experienced
- Number of “mindless” eating episodes
- Apparently irrelevant behaviors (behaviours that, at first glance, don’t seem relevant to binge eating and purging but that actually are important in the behavior chain leading to these behaviors)
- Capitulating (giving up on your goals to stop binge eating and to skillfully cope with emotions)
- Level of food preoccupation
Dialectical Abstinence
This technique is introduced in session 2.
It involves a discussion between the therapist and client, where the therapist tries to get a total commitment from the client to achieve abstinence and to commit to relapse prevention strategies.
This isn’t to say that people will stop binge eating/purging immediately after this commitment.
So, if a person still engaged in binge eating, then the emphasis changes to radical acceptance, non-judgemental problem solving and effective relapse prevention, followed by a speedy return to unrelenting insistence on abstinence.
Urge Surfing
Urge surfing is another core DBT component.
It involves mindful, non-attached observation of urges to binge or to eat mindlessly.
Clients are taught about how urges and cravings are classically conditioned responses that have been associated with a particular cue.
Mindful urge surfing involves awareness without engaging in impulsive mood-dependent behavior.
One learns to “let go” or “detach” from the object of the urge, being fully in the moment, “riding the wave” of the urge and noticing its ebb and flow.
Burning Bridges
Burning bridges is a radical acceptance skill that involves accepting at the deepest and most radical level the idea that one is really not going to binge eat, mindlessly eat, or abuse oneself with food ever again.
One accepts that they will no longer block, deny, or avoid reality with binge eating.
Instead, one makes a commitment from deep within to accept reality and one’s experiences as they are.
Alternative Rebellion
This technique involves being effective in satisfying a wish to rebel without destroying one’s overriding objective to stop binge eating.
The purpose is not to suppress or judge the rebellion but to find creative ways to rebel.
Many clients with BED have described the desire to “get back” at society, friends, and/or family perceived to be judgmental about their weight. For these clients, “getting back” often involves rebelling by consuming even more food.
This isn’t effective, though.
Therapists can encourage clients to observe the need to rebel, label it as such, and then, if the decision is to act on the wish, to do so effectively.
Clients can be creative in thinking up alternate rebellion strategies.
For example, a client who feels judged by society for being obese might “rebel” by mindfully sitting in a well-regarded restaurant and openly, unselfconsciously treating herself to a healthy and delicious bowl of soup.
Is Dialectical Behavior Therapy Effective?
The evidence supporting the effectiveness of DBT for eating disorders is growing.
There have been many different research studies that have evaluated DBT 4Safer, D. L., Robinson, A. H., & Jo, B. (2010). Outcome from a randomized controlled trial of group therapy for binge eating disorder: comparing dialectical behavior therapy adapted for binge eating to an active comparison group therapy. Behavior Therapy, 41, 106-120 5 Chen, E. Y., Cacioppo, J., Fettich, K., Gallop, R., McCloskey, M. S., Olino, T., & Zeffiro, T. A. (2016). An adaptive randomized trial of dialectical behavior therapy and cognitive behavior therapy for binge-eating. Psychological Medicine, 47, 703-717.
Let’s briefly summarise the key findings from DBT studies:
- 56% of people with binge-eating disorder completely stop binge eating after DBT
- 27% of people with bulimia nervosa completely stop binge eating and purging after DBT
- DBT results in quicker reductions in binge eating than some standard group therapy
- DBT can produce reductions in eating disorder symptoms that are sustained a year after treatment
DBT and CBT are equally effective for people with bulimia nervosa and binge eating disorder who don’t respond to an earlier self-help therapy
Useful Dialectical Behavior Therapy Books
I’ll finish off this article by providing some very useful books which clearly talk about, explain, and describe DBT and its underlying, techniques, structure, and components.
If you’re interested in learning more about DBT, then I’d highly recommend getting your hands on the following books
- DBT? Skills training manual (2014): Guilford Publications. Marsha Linehan
- Dialectical behavior therapy with suicidal adolescents. Guilford Press, 2006. Miller, Alec L., Jill H. Rathus, and Marsha M. Linehan.
- Dimeff, Linda A., and Kelly Ed Koerner. Dialectical behavior therapy in clinical practice: Applications across disorders and settings. Guilford Press, 2007.
- Linehan, Marsha M., Bryan N. Cochran, and Constance A. Kehrer. “Dialectical behavior therapy for borderline personality disorder.” Clinical handbook of psychological disorders: A step-by-step treatment manual 4 (2001)
Hopefully, this article answered some pressing questions you might have had about DBT treatment.
As we’ve touched on, there is a heap of options available, and each seems to “work” to some extent.
While there is some evidence to suggest that some approaches work better than others, it’s important that you find out what works best for you.
References

Leave a Reply